Interoperability : Definition, Goals and Benefits
Originally posted on https://www.revenuexl.com/interoperability
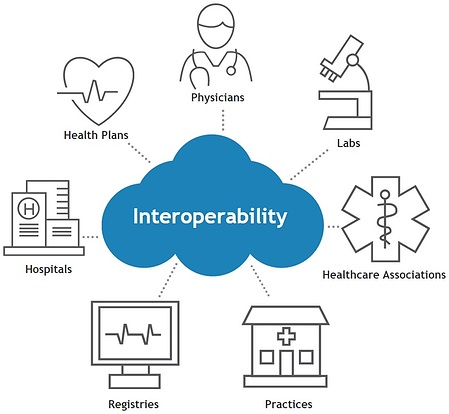
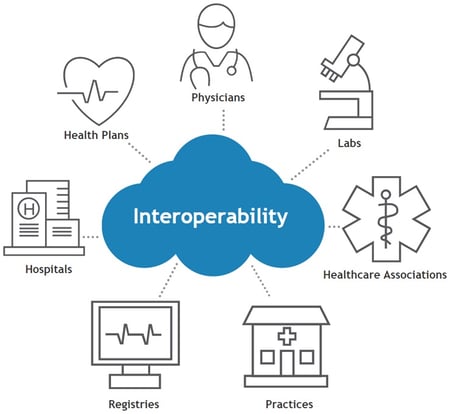
In healthcare, interoperability means the ability of health information systems, devices or software applications to connect and work together within and across organizational boundaries in order to advance the effective delivery of healthcare for individuals and communities. It is achieved through the use of data exchange schema and standards that permit data to be shared across clinicians, lab, hospital, pharmacy, and patient regardless of the application or application vendor.
Role of Interoperability In Healthcare
Interoperability is a process that allows for the seamless exchange of electronic health information between systems (internal and external) without any special effort necessary by the end user. It is designed so that clinicians can provide higher-quality patient care, coordinate care between clinicians and standardize public health data collection/reporting. The goal of interoperability is to provide better  health management and patient outcomes and enhance patient safety and operational efficiency with the reduction of duplicated effort and potential for errors.
health management and patient outcomes and enhance patient safety and operational efficiency with the reduction of duplicated effort and potential for errors.
Under ideal conditions, interoperability facilitates connections and integration across all different types of systems. This exchange of information should occur regardless of where the data originates, its target end user (including the patient) or the applications used. It also needs to ensure that the data that is being transmitted and received are usable and immediately available to share. If this process is operating correctly, it acts as a key element for clinical decision support systems.
Types of Interoperability
Systems not only need to have the ability to exchange information, but they must also be able to interpret and present the information to the recipient in an intelligent way. Each component, as defined by the HIMSS, demonstrates the types of exchange that different organizations may participate in, as well as data sharing that may occur concurrently within an individual setting. This three-tiered modelincludes:
Foundational Interoperability
This is the initial tier of data sharing between disparate systems. It ensures that one software system has the ability to connect to a separate software system in order to share and receive data between the two. It does not take into account the ability of the receiving system to be able to interpret the data without technologies.
Structural Interoperability
This intermediate tier defines the structure or format of data to be exchanged. There should be a standard or uniform exchange of healthcare data from one system to another. This is also known as syntactic or technical interoperability and it ensures that sharing can be interpreted at the data field level. With this, the HIMMS states that “the clinical or operational purpose and meaning of the data must be preserved and unaltered”.
Semantic Interoperability
This highest tier ensures the ability of two or more systems to share, interpret and use the information that is exchanged. Semantic interoperability utilizes both the structuring and codification of the data (including standard vocabulary) in order to support the electronic exchange of patient data and information. In healthcare, semantic interoperability is vital to potentially eliminate the technology and terminology gaps that currently exist between the numerous software systems and data sources.
Goal(s) of Healthcare Interoperability
The ultimate goal of healthcare interoperability is to accomplish the goals established under the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 and reinforced by the Shared Nationwide Interoperability Roadmap.
 Enable Greater Efficiency
Enable Greater Efficiency
When data are presented in a consistent and well-organized manner (regardless of the source) it is far easier for clinicians to quickly access it, evaluate, and determine the cause of the patient issue while they make treatment decisions. This process becomes even easier when the same clinicians are provided with technological solutions that assist them when making those decisions.
Better Patient Engagement
When we consider the goals of interoperability, healthcare is ultimately about empowering providers to achieve better patient outcomes. However, we are also empowering the patients with information and knowledge for them to take an active role in their own care.
For nearly a decade, we have been progressively moving toward Meaningful Use. Despite some beliefs, the goal has always been aimed at improving patient care and improving access to patient information. This IT integration allows providers to put personal health information directly in the patients’ hands. This can now be accomplished as a far easier task (i.e. patient portals) and it can be accomplished sometimes in a matter of hours, where it used to take days by phone or weeks by mail.
This alone has dramatically contributed to the improvement of health in our practices and communities. Practitioners can follow-up with patients far quicker than in the past, affording them and the patient to take the next step(s) in the process of diagnoses, provide continuity of care with referrals or reinforce items related to their treatment plan.
Improve ROI
One of the greatest incentives for interoperability is the necessity to recover a portion, if not all, of the cost associated with the required implementation of new technology. Any practice or clinical office appreciates a substantial return on investment. When you have invested in new technology, you deserve to get the full value out of it, and it is even better if you can get a positive net income from your investment.
Benefits of Interoperability
Reduces Errors and Improves Efficiency
By integrating new software systems into your practice/clinical site, you have the ability to streamline certain processes, eliminate much of your manual data entry, minimize errors, and free up time for other tasks within the office. With connections to health information exchanges (HIEs) and electronic health records EHRs, your interoperability capabilities can not only help to improve practice efficiency, but it can ensure your compliance with pay-for-performance initiatives (MACRA/MIPS), the Cures Act, etc. Therefore, as long as data is initially entered correctly, your practice/office stands a greater chance of accurately storing protected health information (PHI) for an entire life cycle.
it can ensure your compliance with pay-for-performance initiatives (MACRA/MIPS), the Cures Act, etc. Therefore, as long as data is initially entered correctly, your practice/office stands a greater chance of accurately storing protected health information (PHI) for an entire life cycle.
More Accurate Reporting (Data and Trends)
The ideal situation would be one in which every healthcare provider/office would be interoperable with one another, as outlined in the goals of the “Roadmap”. This would create a single network of shared data across North America. All data pertaining to patient health care could be shared with any eligible provider, laboratory, diagnostic center, hospital, etc., and we would be able to use this data to predict long-term health trends.
Interoperability provides digital health information with technologies that can facilitate quicker and more a precise collection of public health data. This, in turn, can be used to recognize, interpret, track and predict the spread of contagious diseases. With this information, public health agencies could effectively enable better preparation, limit their spread and increase the efficacy of treatments.
This same data that is collected, could be applied to non-contagious diseases (NCD) and aid in predicting long-term health trends (in real time) across the country. This could allow for additional opportunities to address these NCDs and create strategies for preventative measures to be adopted on a far larger scale. This, in turn, could potentially help to reduce the long-term cost associated with the care of these populations.
Better Access to More Complete Patient Records
Patients tend to go to various different places for their healthcare. Not every type of healthcare setting is going to capture the same data, nor are all of them going to be connected electronically. When we consider all of the different offices a patient might visit (primary care, specialists, dental, ophthalmic, OT, PT, chiropractic, school clinics/nurses, etc.) it is unlikely that every form of healthcare will ultimately be part of one HIS.
What we can anticipate is that someday, there will be interoperability of these systems to connect with each other, and securely share data. Then we will have the opportunity to populate a more complete patient record and provide continuity of care, particularly for complex cases. The immediate goal isn’t to have just one system that does everything, but to get all forms of healthcare connected to the information that exists.
Improves Patient Safety
We have all seen what happens when secure information is breached. It has happened in nearly every industry and when practices/offices do not know exactly where their patient data exists, privacy breaches are bound to be a reality. No matter how precise your standard operating procedures are, you cannot guarantee that a note containing PHI on a piece of scrap paper will be appropriately discarded and not unintentionally tossed in a full trash can in an unsecured area. However, when sensitive data is input via a secure interoperable network, you can be ensured that the patients’ PHI will be properly protected.
When patient data exists in a variety of locations, it seems almost improbable that you will have access to complete patient records. Manual data input errors can be made very easily, and a patient’s health and safety could be at risk. Interoperability ensures your systems and EHR-based CDS, provide the best patient-care experience and patient outcomes possible.
Current State of Interoperability in Healthcare
Electronic data and healthcare IT (HIT) systems have grown rapidly throughout the last decade. But it seems that these technological innovations have developed in isolated regions of the country and specific areas of the healthcare industry. The initial surge of HIT development took place in billing and claims. The next phase included localized improvement of ancillary clinical systems (laboratory, pharmacy, and radiology). These were then followed by the inclusion of administrative services. More recently, the healthcare industry’s emphasis has shifted to electronic health record (EHR) systems.
At this time, many of the healthcare systems and clinical practices across the country, have established IT systems independently of one another and continue to exist primarily as isolated entities of automation. It is understood by most, that communication is one of the most urgent technological issues that the healthcare community struggles with today. Reducing the communications gap has become extremely important. As healthcare institutions continue to launch new software systems in order to improve their own patient outcomes and improve operational efficiencies, the need for those systems to be able to communicate with each other will ultimately continue to grow.
In addition, communication is essential to the emerging healthcare industry and new healthcare delivery models. For example, accountable care organizations (ACOs) and patient-centered medical homes (PCMHs), depend highly on the ability to share data among primary care physicians, specialists, hospitals and insurance providers. Many healthcare managers feel that interoperability is the cure for the lack of communication that currently exists among disparate systems. This area of healthcare technology incorporates multiple tiers of communication that healthcare providers need to understand.
Future Interoperability Trends to Watch
The urge to digitize healthcare has been going on for at least 10 years. This began was with the initial force for hospitals and physicians to begin implementation of EHRs. Now, years later, these providers are searching for new ways to attain measurable results with the current systems that are already in place.
Updated federal regulations based on annual reports and new roadmaps, artificial intelligence (AI), growing choices for interoperability networks, and increases in patient data access opportunities are all high priority healthcare interoperability areas that are likely to impact the industry in the coming years.
Changing Federal Regulations
The U.S. government, through the HIMSS Interoperability Initiatives, the Federal Health IT Strategic Plan 2015-2020, the Shared Nationwide Interoperability Roadmap, and Promoting Interoperability (PI) has placed interoperability in the forefront of what they feel is critical for the emerging healthcare industry. They have identified HIE as a critical part of interoperability and require hospital and medical providers to meet all of the federal and state requirements found in the legislative initiatives outlined in the American Recovery and Reinvestment Act of 2009 (ARRA), MIPS, APMs, etc. It has become an “alphabet soup” that many providers feel that they are drowning in.
The latest changes have come about with the Promoting Interoperability Programs (PI). The CMS IPPS/LTCH PPS final rule (CMS-1694-F) includes new provisions for payment and policies. In addition to these, CMS revamped the Medicare and Medicaid Promoting Interoperability Programs in order to better achieve program goals. This rule confirmed an EHR reporting period to be a minimum of any continuous 90-day period in each of calendar years 2019 and 2020 for new and returning participants working with CMS or their State Medicaid agency.
Patient Data Access Further Pushes Interoperability
Pressure is mounting for providers to increase the efficacy of digital patient information sharing across critical systems and the functional teams that use them. It is believed that enabling this increase in efficiency will positively affect patient care and enhance clinical decision support.
The ONC’s interoperability goals include:
- Patients must be able to access their health information electronically without any special effort
- Providers and payer organizations responsible for managing benefits can receive population-level health information allowing them to analyze health trends, outcomes, and costs
- Identifying at-risk populations, and track the progress of quality improvement initiatives
- The health IT community should have open and accessible application programming interfaces (APIs) to encourage entrepreneurial, user-focused innovation to make health information more accessible and to improve electronic health record (EHR) usability.
Many believe that increased interoperability can boost value-based care, patient demand for data sharing and improved interoperability will have the added side-effect of propelling industry-wide momentum toward value-based care in 2019. Currently, the lack of interoperability has historically suppressed this growth.
Interoperability for Small Healthcare Practices
 When looking at what has been accomplished in healthcare in general, and in healthcare IT, over just the last 10 years, the sweeping changes and regulations have given rise to a host of new technologies and methodologies that allow clinicians to partner and share data more than ever.
When looking at what has been accomplished in healthcare in general, and in healthcare IT, over just the last 10 years, the sweeping changes and regulations have given rise to a host of new technologies and methodologies that allow clinicians to partner and share data more than ever.
ONC, through their Roadmap, plans to incentivize providers to implement and use the resulting interoperability data standards in patient care. As they plan to use the Roadmap as a “living document”, there will be changes and clarifications made to interoperability standards and goals over the next few years. Provider organizations, including small group practices, stand to reap tremendous benefits from using such interoperability as described in the Roadmap. Some of these benefits include:
- Improved patient health outcomes
- Improved health care quality
- Lowered health care costs
- Tailored treatment recommendations that account for each patient’s individual genetics, preferences and health history
- Increased patient engagement
- Greater competition among EHR vendors
- Reduced redundancy
This Roadmap and the other federal and state regulation (that are continuously changing) can be overwhelming for small practices and clinical offices. However, the ONC has made specific provisions for small practice/office owners when it comes to HIN implementation.
Smaller practices/offices are permitted to join with other like-minded groups to utilize a collective bargaining power related to implementation and use of new technologies, standards and best practices required for interoperability. They can also take the option of joining an HIE (local or statewide) that can offer the scalability and security that a small practice/office may need in order to remain cost-effective while transitioning into new technologies.
Looking Ahead
The ever-changing and technologically advancing field of medicine poses specific challenges for the role of interoperability for small practices and medical providers. Regardless of the size of the practice, federal and state regulations apply to all. This push to share data is close to reaching its goal, but there are bumps in the road for some providers. Even though the technical means exist, not all providers are using interoperable technology components. A large part of this is due to the lack of resources that smaller and single practices have. However, many of these providers are realizing that interoperability is a key strategy for maintaining independence.

